U.S. Sen. Bob Casey this week introduced a bill that would lower costs for people who need drug addiction treatment. Another Pennsylvania Democrat, U.S. Rep. Madeleine Dean, said she would introduce a similar bill in the U.S. House.
What would the bills do?
Mainly, they would eliminate insurance deductibles and co-pays for prescription drugs used to treat opioid addiction and for behavioral health services during treatment and recovery.
The provisions would apply to private insurance coverage and Medicaid, which covers people with lower incomes.
Why does it matter?
According to Casey, 20 million Americans have opioid use disorder and 115 people per day are dying from it. The long-term costs of treatment are a barrier to recovery, he said.
A bill summary from Casey and Dean says: These provisions draw from proven models that have demonstrated increases in treatment success in various states, including [medication assisted treatment] cost-sharing elimination and copayment assistance for naloxone. Further, the use of peer providers, people who are also in recovery from substance use disorders, shows great promise to help people new to recovery and bolster behavioral health workforce numbers.
Who else is behind it?
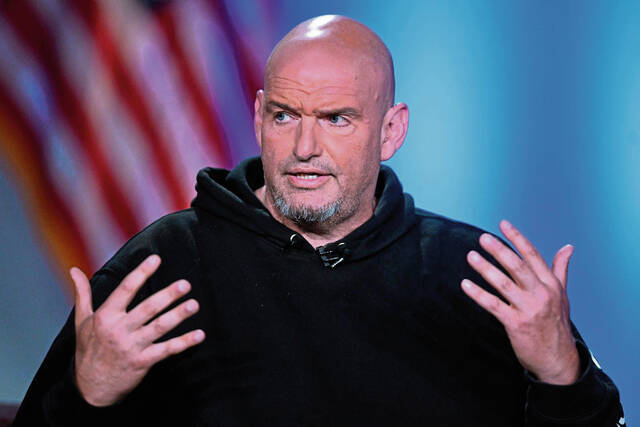
A news release from Casey named these co-sponsors: fellow Democratic senators John Fetterman of Pennsylvania, Amy Klobuchar of Minnesota and Richard Blumenthal of Connecticut.
How severe is the problem in Pennsylvania?
Pennsylvania had about 5,120 fatal overdoses during the 12 months ending last October, according to the latest federal estimate.
That’s about 300 fewer than in 2021, but still nearly 700 more than in 2019, when it seemed Pennsylvania had turned the tide against fatal overdoses.