Francis Regis Johns IV was born at 8:50 a.m. Jan. 10.
By 8 p.m. on Jan. 11, he was comfortably at his Greensburg home.
“He was good, and I was feeling good, so the best option was to come home,” said Francis’ mother Sarah Johns.
UPMC Magee-Womens Hospital in Oakland is giving new moms the option to leave earlier than what has historically been the normal stay.
It’s a plan administrators put in place during the coronavirus pandemic.
They are considering offering it once life returns to some normalcy after covid-19.
Some women can now be discharged at the 24-hour mark following a vaginal delivery and 48 hours for a c-section.
Different experiences
The experience with having her son was different for Johns than when her first child, Jennica, 2½, came into the world.
She and the baby spent five days in the hospital.
A sizable percentage of moms have chosen to go home early, said Dr. Richard Beigi, president of UPMC Magee.
The hospital is averaging a half-day earlier length of stay since the option to shorten the time was put in place.
Before that, it was 48 hours for a vaginal delivery and 72 for a cesarean section. The average stay then was one-and-a-half days for a vaginal delivery and two-and-a-half days for a cesarean section.
Johns said she would have left several hours earlier, but there were paperwork issues.
Beigi said some women will need to stay longer, whether it is because of high or low blood pressure, bleeding, infection or personal reasons.
When to leave is a discussion between the care team and the patient, Beigi said.
“In the face of covid, we set out to do this,” Beigi said. “If they don’t have any complications, they can go home if they want. We want to give them the choice.”
The shorter stays shouldn’t affect medical insurance coverage because patients are staying less time and not more, Beigi said.
“We’ve received lots of favorable responses,” Beigi said. “Most of them don’t need to stay that long. If a baby is doing well here, there is no reason to think the baby won’t do well going home early.”
Research results
The results at Magee are in line with what a study about shorter hospitalization stays found. Researcher Naomi H. Greene and doctors Sarah J. Kilpatrick, Melissa S. Wong, John A. Ozimek and Mariam Naqvi at Cedars-Sinai in Los Angeles, Calif., focused on deliveries between Jan. 1, 2020, and April 30, 2020.
Obstetricians, maternal-fetal medicine specialists, pediatricians, anesthesiologists, infectious disease specialists and nursing leadership were involved in the project.
They looked at the first two months, which were before the modifications were made for shorter hospitals stays. They compared those first two months to discharges in March and April.
They found that “maternal and newborn length of stay in the hospital were significantly shorter after delivery without increases in the rate of adverse maternal or neonatal outcomes.”
They acted after the Society for Maternal-Fetal Medicine and Society for Obstetric Anesthesiology and Perinatology issued guidelines on safe delivery and obstetric care during the covid-19 pandemic. The piece was published in the American Journal of Obstetrics & Gynecology Maternal-Fetal Medicine.
The family unit
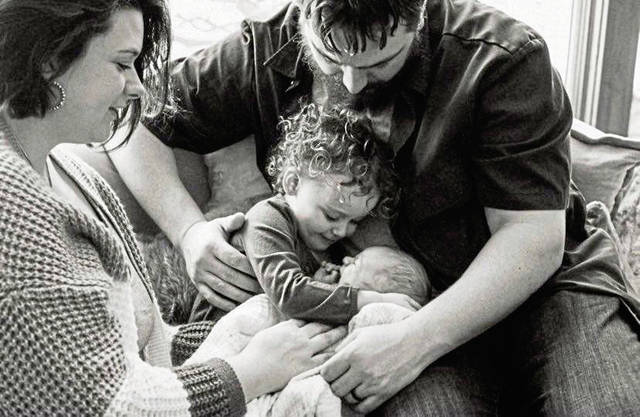
A big reason to leave early was to be home with Jennica. Sarah Johns and husband Francis Regis Johns III wanted time together for their family.
“We wanted a peaceful few moments when our daughter could meet her little brother,” Sarah Johns said.
Sarah Johns said she wasn’t concerned about covid-19 and was confident the hospital had all the safety measures in place.
Hospitals have instituted other guidelines concerning care because of the virus. One is limiting the number of people who accompany a patient. Having that time with her husband and their newborn helped the three of them bond and allowed her to concentrate on learning about caring for her baby.
“The doctors and nurses and everyone at Magee were wonderful,” Johns said. “They made sure we were fine to leave. They are so calm, and they know how to make you feel at ease.”
Advancements in technology
Beigi said there are better ways to stay in contact with a new mom through technology — from text messages from nurses and staff to virtual doctor visits.
The hospital has a remote-monitoring program for pregnant and postpartum women with hypertensive disorders. It uses an app to communicate with her care team. Many women are opting for prenatal telemedicine appointments and are utilizing virtual visits for their six-week postpartum checkup, according to the UPMC.
Patients are provided a blood pressure cuff to help with at-home monitoring for their prenatal telemedicine appointments. It prompts women to take their blood pressure, which, along with their heart rate, are recorded via an app.
With fewer visitors, moms can receive the instruction they need, such as breast feeding sessions to other details about caring for a newborn, more quickly because there aren’t interruptions.
“With covid rules, there is only one person allowed in the room,” Beigi said. “That’s a huge benefit to the nurses and doctors, who can devote their time to the patient and her baby. “
Both of Johns’ babies were vaginal deliveries.
Jennica was 8 pounds, 2 ounces and 21 ½ inches long, and Francis IV was 8 pounds 15 ounces and 21 inches long.
“I felt comfortable leaving,” she said. “I didn’t feel like we were getting evicted. We feel great at home. Hospital beds aren’t that comfortable.”