https://development.triblive.com/local/pittsburgh-allegheny/university-of-pittsburgh-launches-trials-of-coronavirus-drugs-including-hydroxychloroquine/
UPMC launches trials of coronavirus drugs, including hydroxychloroquine
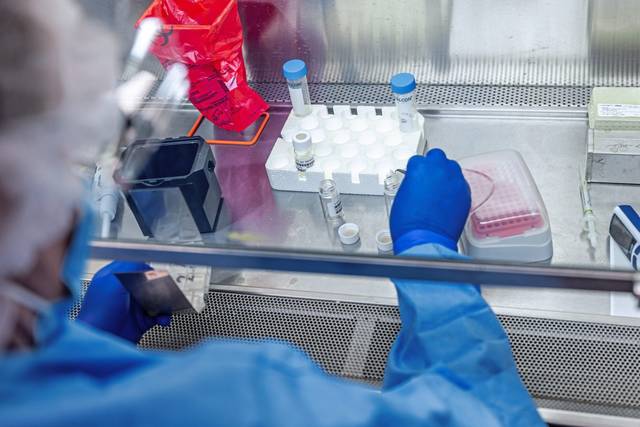
Researchers at the University of Pittsburgh School of Medicine and UPMC on Thursday launched a new, global effort they say could speed up the process for testing covid-19 treatments.
“We don’t have the luxury of time,” Dr. Derek Angus, UPMC chair of critical care, said during a news conference.
Multiple covid-19 treatments will be tested in different combinations, including the anti-malarial drug hydroxychloroquine, steroids and medications called immunomodulators that alter the responsiveness of the immune system.
There are no drugs approved by the U.S. Food and Drug Administration to treat covid-19, the disease caused by the novel coronavirus. While hydroxychloroquine has received a lot of attention lately, Angus said researchers still don’t know if it will be the best treatment.
“I don’t know what will work best,” Angus said. “I have personal hope that some of the antivirals will help a little bit, but I think we will also need to help the immune system have a more favorable response. The correct answer is probably going to be a combination of therapies that we haven’t even tried.”
The effort builds on a testing method developed by an international team of researchers before the novel coronavirus outbreak. That method, called REMAP-Community Acquired Pneumonia, or REMAP-CAP, was designed to find treatments for severe pneumonia but has since been adapted for evaluating treatments specifically targeting SARS-CoV-2, the virus that causes covid-19.
Those findings were published Thursday in Annals of the American Thoracic Society, or AnnalsATS, a medical journal highlighting research in the fields of pulmonology and critical care medicine.
Unlike traditional clinical trial testing, this method uses machine learning to track several treatment options simultaneously, allowing doctors to adjust combinations of therapies or to discontinue those that are not effective more efficiently.
“This allows us to always rapidly identify which treatment works best, while keeping the number of patients needed to achieve statistical significance low,” Angus said. “It also means we get the best treatment to the most patients right out of the gate.”
This method also could test treatments at a lower cost and using fewer patients, researchers said.
The trial conducted at UPMC, called UPMC-REMAP-COVID19, will open across the 40-hospital UPMC system and will be integrated into the health system’s record system. Any covid-19 patient admitted to a UPMC hospital for treatment will be eligible to participate in the trial.
The data also will be connected to the global REMAP-CAP, which will include information collected from covid-19 patients throughout North America, Europe, Australia and New Zealand.
Unlike traditional clinical trials, which would test each drug individually, additional drugs will be rolled into this testing system as needed.
“In a pandemic, doctors will not have the time to debate the pros and cons of every possible clinical trial,” Angus said. “By building this one-stop solution at the point of care, we are rolling out an approach that can assure that every patient admitted with covid-19, if they choose to, can be enrolled in the program.”
In addition to receiving the current standard of care, most patients would receive at least one of the experimental treatment options if they choose to enroll in the trial, according to a statement from UPMC.
At launch, about 12.5% of participants will be assigned to the placebo arm of the trial. Researchers expect that about 99% of patients will be receiving one or more active therapies within weeks.
It’s not yet clear how soon the trial will yield results that show, with certainty, which treatments work best.
This will depend on how many patients enroll in the program, Angus said.
The design and implementation of the UPMC-REMAP-COVID19 trial is led by Angus and colleagues at Berry Consultants (Austin, Texas), and supported by UPMC Enterprises.
Copyright ©2026— Trib Total Media, LLC (TribLIVE.com)
